Top six common questions about pregnancy, answered by Fertility Specialist and OBGYN Dr Iris Wang.

If you are currently trying to fall pregnant, or you have recently received happy news that you’re expecting, you might have questions around pregnancy and what to expect – how many doctors’ appointments will you need to go to? What about morning sickness? Can you still exercise at the same intensity level?
Dr Iris Wang, fertility specialist and OBGYN at IVFAustralia, provides expert insight on six of the most common questions about pregnancy.
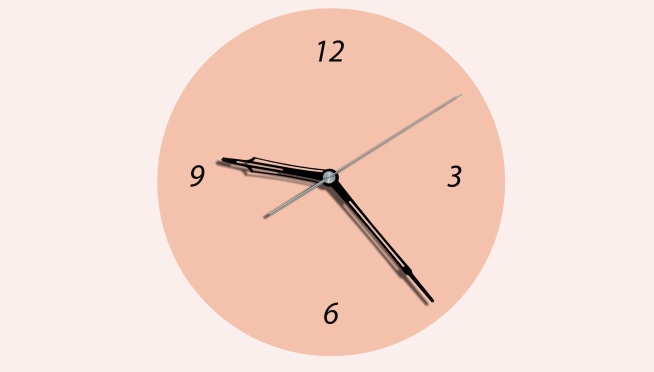
- How is the due date determined?
The due date is calculated by 40 weeks from the first day of the last normal menstrual period. This is on the basis that the period is a very standard 28 day cycle. Which means, it is actually 38 weeks from conception.
If you aren’t sure when your last period was, an ultrasound can help determine the due date after the first 6 weeks of pregnancy.
- What do you suggest to combat morning sickness? How long should I expect morning sickness to last?
Morning sickness really does vary for each individual. Some women don’t experience morning sickness at all, while a few will have severe morning sickness.
Unfortunately as evidence based medicine goes, there’s not much you can do. However, you might find that natural remedies are helpful, for example ginger or multivitamins like B6 and B1. Some foods can bring on feelings of nausea more than others, and I always tell my patients to approach it with a ‘trial and error’ mindset to see what really works for you.
And then once you get to 16 weeks, this is usually a turning point. Most women feel better after this, with morning sickness dissipating. It’s very rare for it to continue past 16 weeks.
- How many times do I need to see the doctor during pregnancy?
Generally speaking, it will work out to be 10 – 12 times. Most doctors will see the patient by about 10-12 weeks. You’ll then start to see the obstetrician from about week 10. From there, tests will be organised and arranged to monitor your health and the baby’s health.
There will be visits every 4-6 weeks up to 28 weeks, and then every 2-3 weeks up to 36 weeks. From week 36, it’s likely weekly visits.
This may vary, of course, depending on your health and the baby’s health.
- What happens at prenatal appointments?
Prenatal appointments involve:
- Taking your blood pressure
- Checking your weight
- Taking a urine sample to check for too much protein (a possible sign of preeclampsia) or sugar (a possible sign of gestational diabetes)
- Checking for swelling in your hands, feet or face
- Listen to your baby's heartbeat (from week 16 on, though it can be heard on a Doppler device as early as week 10)
- Measure and feel your belly to check your baby's size and position (in the second and third trimesters). Usually, it’s not very easy to feel how the baby is lying until 27 – 28 weeks.
- What exercise is okay for me to continue during pregnancy?
Exercise is encouraged to continue for general health and fitness while pregnant, both in terms of avoiding too much weight gain as well as benefiting your emotional wellbeing.
If you already exercise regularly, you may continue to do so with a little bit less intensity. I typically recommend to do 80% of what you normally do.
- Speaking of weight, do I need to ‘eat for two’ while pregnant?
This is actually a common misconception. You should continue to eat a healthy, well-balanced diet during pregnancy, adding an additional 350 – 450 calories per day. For example, adding a few healthy snacks throughout your day such as carrots and hummus, a fruit salad, or hard-boiled egg.
It can also depend on your current weight, height and trimester of pregnancy so be sure to speak to your doctor about this.