Meet Professor David Gardner, an IVF pioneer and world-renowned scientist, as well as Virtus Health’s Group Director of ART, Scientific Innovation & Research. Prof Gardner is one of the most highly cited scientists in reproductive medicine and a Fellow of the Australian Academy of Science.
Much of David’s research has been successfully translated into clinical procedures, with the majority of human IVF clinics around the world utilising some of the technologies he developed. As the namesake of blastocyst grading, the internationally used 'Gardner scale’, Prof Gardner has made significant contributions to the field of Reproductive Medicine for over three decades, and is well known for his pioneering work on the development and clinical introduction of blastocyst transfer.
And now, under Prof Gardner’s leadership, Virtus Health has introduced a new initiative called OneLab, a strategy designed to set a new benchmark in the delivery of scientific services for patients hoping to achieve their dreams of parenthood.
Here, we speak with Professor Gardner about the OneLab strategy, and the inspiring future of reproductive medicine.
How would you describe the OneLab initiative in your own words?
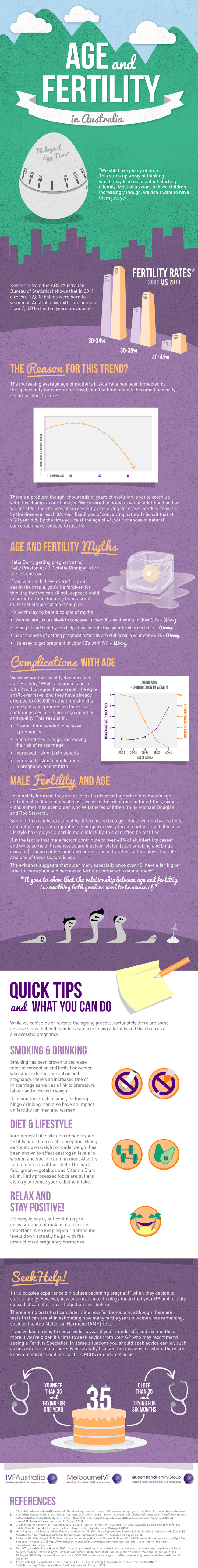
The OneLab strategy is based upon utilising the extensive collective experience and expertise that resides across the Virtus Health clinics (including IVFAustralia, Melbourne IVF, Queensland Fertility Group and TasIVF) to both optimise and standardise all laboratory procedures. Through such a collegiate and collaborative approach we have been able to make significant improvements in the laboratory and increase patient outcomes, and subsequently translate this success nationwide very quickly.
OneLab is designed to set a new benchmark in the delivery of scientific services to our patients.
What inspired you to create the OneLab strategy for improvement?
The IVF laboratory is an extremely complex environment, utilising numerous specialised technologies required to attain our goal of converting as many couples into families as possible. We therefore wanted to ensure that all patients attending a Virtus Health clinic received the same chance of conceiving.
What are the top 3 elements integral to achieving this new benchmark?
Procedures, technology and lab design. These are the top 3 areas we have focused on;
- Improving how laboratories are run.
- Introducing new equipment (such as time-culture combined with Artificial Intelligence -AI) to enhance embryo development and improve selection for transfer, resulting in not only more pregnancies, but establishing pregnancies quicker.
- Building the next generation IVF laboratories for increased efficiency and effectiveness.
What motivates you as a scientist and embryologist, and what do you find exciting about the future of this field?
I have been a scientist working in embryology and IVF for 40 years and have seen many technologies introduced which have greatly increased the success of human IVF. When I started out, implantation and clinical pregnancy rates were less than 10% and consequently several embryos were transferred to try and increase success. This approach did marginally increase success rates, but with also introduced the problems associated with multiple gestations (twins, triplets, etc.), resulting in pregnancy complications. With advances in culture technologies, driven largely by my own lab which developed and introduced blastocyst culture, we can now attain implantation and clinical pregnancy rates of around 50% in patients under 38 years, and only need to transfer a single embryo.
What is coming to the field of human IVF is a greater use of AI to assist in all aspects of patient care and treatment, combined with new technologies in both genetics and in microfabrication - the so called Lab in a Box. The former will assure the transfer of chromosomally normal embryos while the latter will lead to new and improved methods of IVF and embryo culture. Further, new non-invasive analysis of biomarkers of embryo health (determined by analysing spent culture media) will assist is identifying the best embryo for transfer. Finally, ongoing research into the next generation of culture media will provide the opportunity to increase pregnancy rates.
Based on your experience, what do you think is important for patients to look for in their fertility clinic’s laboratory?
A commitment to excellence, and the development and introduction of new technologies to maximise the chance of success for every cycle of IVF performed.